Underlying mutation, sleep problems tied to anxiety, depression in Rett
Better managing sleep in clinic may help improve mental health: Study
Written by |
Levels of anxiety and depression in girls and women with Rett syndrome are influenced both by the individual’s type of MeCP2 gene mutation — the underlying cause of the neurodevelopmental disorder — and the presence of sleep problems, a new study reports.
In particular, patients carrying p.Arg294*, a mutation usually linked to milder Rett disease, were found to have more anxiety but comparable depression to those with a severe mutation called p.Arg270*. Also, insomnia and excessive daytime sleepiness were associated with higher levels of anxiety and depression.
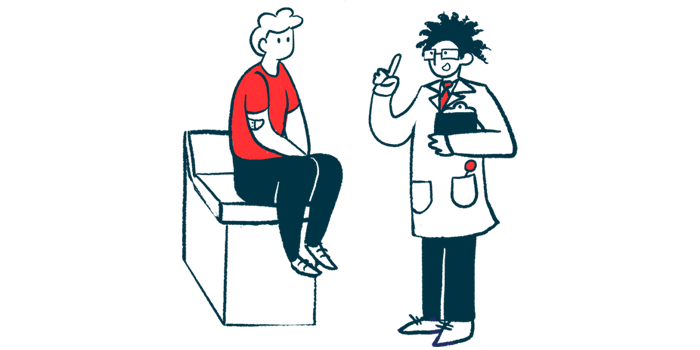
These findings highlight that both MeCP2 mutation type and sleeping issues are independent predictive factors of mental health in Rett patients, according to the researchers.
“Sleep difficulties were associated with poorer mental health, indicating the importance of routine evaluation and management of sleep in clinical care,” the team wrote, noting that their findings suggest that “proactive management of poor sleep could improve mental health.”
The study, “Genotype and sleep independently predict mental health in Rett syndrome: an observational study,” was published in the Journal of Medical Genetics.
Research seek new ways to improve mental health
Affecting females almost exclusively, Rett syndrome is mostly caused by mutations in the MECP2 gene. The resulting MeCP2 protein regulates the activity of other genes and is involved in nerve cell function and communication.
MECP2 mutations lead to lower-than-normal levels of MeCP2 or the production of a faulty protein, which typically result in symptoms such as motor and cognitive problems — but sometimes also mental health and behavioral issues.
Rett’s clinical spectrum “is broad and is in part influenced by the specific underlying [mutation],” the researchers wrote.
Of particular focus in this study was the p.Arg294* mutation, which generally is linked to less severe symptoms among patients. However, previous studies have shown that individuals with Rett who carry the p.Arg294* mutation “have more sleep disturbances and have the poorest quality of life,” the team noted.
“Previous research has focused on physical comorbidities [coexisting conditions] with comparatively little research on mental health and behaviors,” the researchers wrote, adding that earlier investigations into mental health focused mainly on anxiety/fear and less on depression.
With that in mind, the team here — from the University of Western Australia — evaluated mental health with a specific emphasis on anxiety and depression. Their study sought potential predictors of poorer mental health in 210 girls and women with Rett, ages 6-51.
All patients were enrolled in the International Rett Syndrome Phenotype Database, which was established in 2002 by the International Rett Syndrome Foundation. Most of the participants (94.8%) lived at the parental home, while the remaining 11 patients lived in a group home or community residential unit.
No sleep impairments found for most patients
The mental health of these women and girls was assessed using the Anxiety, Depression and Mood Scale (ADAMS) questionnaire, which was developed for people with intellectual disability. It covers 28 symptoms, to include anxiety, depression, irritability, and apathy. Each symptom is scored from zero to four, with higher scores indicating more severe symptoms.
The questionnaire was mostly completed by the patients’ biological mother (87.1%), followed by the biological father (9.1%); the remainder were completed by other family members.
The most prevalent MECP2 mutations were severe variants, specifically p.Arg255* (13.8%) and p.Arg168* (12.4%). Milder mutations were less common: p.Arg133Cys was found for 7.6% of patients, and p.Arg306Cys in 5.7%.
The p.Arg294* mutation was identified in 6.7% of participants.
More than one-third of patients (34.3%) could walk independently, while 31% required some assistance to walk, and 33.8% could not walk. Nearly three-quarters (71.5%) had epilepsy.
The majority (71.4%) had no sleep impairments. A total of 26.2% had problems falling asleep, as assessed using the Disorders of Initiating and Maintaining Sleep (DIMS) scores.
Patients’ scores in the Disorders of Excessive Somnolence subscales, known as DOES, showed that most (78.1%) did not experience daytime sleepiness, which affected only 17.6% of participants.
About a quarter of patients (25.7%) were prescribed psychotropic medications for anxiety or depression, with most of them (83.3%) taking anti-anxiety medication.
Next, the researchers assessed how general anxiety and depression scores related with patients’ features, such as type of MeCP2 mutation or genotype, functional abilities, and any simultaneous health conditions.
Better sleep management may improve mental health for some patients
The results showed that patients ages 12 and older showed generally lower anxiety scores than did younger patients, indicating that “anxiety became less prominent with increasing age,” the researchers wrote.
Compared with the 5.2% of patients carrying the severe p.Arg270* mutation, those with the milder p.Arg294* variant had significantly higher general anxiety scores, by more than three points. Patients with the milder p.Arg133Cys mutation had slightly higher general anxiety scores.
Anxiety scores were significantly higher, by about 1.5 points, among patients with trouble falling asleep and those with excessive daytime sleepiness, compared with those without such problems.
Also, patients taking medication for anxiety showed significantly higher anxiety scores, by three points, than those who were not.
Proactive management of poor sleep could improve mental health.
The type of MeCP2 mutation was found to have a smaller effect on depression. Patients carrying the milder p.Arg270* mutation had only slightly increased depression scores relative to those with the severe p.Arg294* mutation. In turn, patients with one of the other two most common milder mutations, p.Arg133Cys or p.Arg306Cys, scored slightly lower, indicating less depression.
Patients with sleep problems generally showed higher mean depressed mood scores than those without, but significant differences were only detected for those with excessive daytime, scoring more than 3.5 points higher.
There were no significant associations between patients’ functional status and mental health measures in analyses considering several factors at the same time.
Overall, these “findings indicated that genotype and sleep have implications for mental health in Rett syndrome,” the researchers wrote.
The team called for “anticipatory guidance” for patients with these MeCP2 mutations, noting “individuals with the p.Arg294* variant had the highest anxiety scores.”
Greater efforts also are needed to treat sleep problems, the researchers noted.
“More research is needed to understand the effects of psychometric medications,” they added.