DNA Sequencing Identifies Unusual Genetic Cause of Rett-like Disease in Young Girl
Researchers have identified an unusual genetic variant in the EEF1A gene as the likely cause of Rett syndrome-like disease in a young Australian girl.
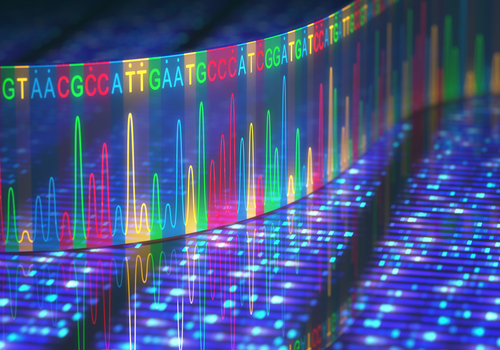
After standard genetic testing failed to identify the cause of her disease, researchers turned to the more advanced whole-exome sequencing (WES) technology to reveal the variant.
The team says this case stresses the importance of using more sophisticated genetic tests to identify the origin of the disease in cases that diverge from classical Rett.
The report, “Whole exome sequencing reveals a de novo missense variant in EEF1A2 in a Rett syndrome‐like patient,” was published in the journal Clinical Case Reports.
Rett syndrome almost always is caused by mutations in the MECP2 gene, and affects females almost exclusively. Some share some of its symptoms, but do not meet all diagnostic criteria for classical Rett. Those cases are considered atypical or “Rett-like” disease.
Although mutations in MECP2 also are the chief cause of atypical Rett, mutations in other genes, including CDKL5 and FOXG1, have been found in patients with overlapping clinical signs.
Researchers from the Murdoch Children’s Research Institute, in Australia, described the case of a 5-year-old girl with Rett-like symptoms that became more evident around age 2.
By that time, she was unable to roll or sit unsupported, could not articulate distinct words, and had limited hand function. She started making stereotypic (purposeless, repetitive) hand movements like hand-clasping and hand‐to‐mouth movements. Her hands and feet were cold and sometimes mottled (blothchy).
She had difficulty eating, as well as constipation, bruxism (teeth grinding) and hypothyroidism, which refers to insufficient production of thyroid hormone by the thyroid gland. The girl also started having seizures, abnormal muscle tone and breathing, as well as inappropriate outbursts of laughter.
At her last visit, at age 5, she continued showing a smaller-than-normal head, as well as significantly low weight (14.3 kg or 31.5 pounds, first percentile) and height (nearly 1 meter or 3.3 feet, first percentile). The girl continued having episodes of breath-holding, developed additional stereotypic hand movements, and showed kyphosis, which is an excessive curvature in the spine sometimes called “roundback.” Meanwhile, her bruxism was not as frequent.
During her follow-up at Children’s Hospital at Westmead, conventional genetic tests could not detect any of the most common disease-causing mutations of Rett. As such, the team decided to use WES, which scans all DNA regions that provide instructions for producing proteins (exons).
Results showed a missense variant — p.(Asp91Asn) — in one copy of the EEF1A2 gene. Missense mutations are changes in the building blocks of DNA, called nucleotides, leading to a different amino acid. In this case, aspartic acid was replaced by asparagine at position 91, the report stated.
Computational modeling then predicted the variant to be damaging and disease-causing.
Atypical variations in EEF1A2 have been associated with neurodevelopmental disorders including epilepsy, autism, and severe intellectual disability, but never with Rett.
The specific mutation present in the Australian girl had been described in a 2016 report about a 14-year-old girl who shared some of the symptoms, such as cold extremities, seizures, low muscle tone, and spine deformity. Other manifestations in that prior case included intellectual disability and inability to walk independently.
“This highlights that a variable neurodevelopmental phenotype [trait] may be associated with EEF1A2 variants, with the same variant resulting in overlapping neurological presentations,” the researchers wrote.
Further tests found that the girls’ parents did not carry the mutation, which means she acquired the genetic change during embryonic development. This is called a de novo (new) mutation.
In addition to confirming the association between EEF1A2 and Rett‐like disease, the researchers said their study also highlights the clinical utility of WES in patients without MECP2 mutations, but whose symptoms are consistent with Rett.
“[W]e suggest that analysis of EEF1A2 should be included in the curation of genomic sequencing data from individuals with a RTT [Rett] or RTT‐like clinical picture,” they added.