Diagnosis of Rett syndrome
Last updated Sept. 19, 2025, by Marisa Wexler, MS

Rett syndrome is a genetic and neurodevelopmental disorder marked by cognitive, emotional, sensory, and motor disturbances. Specialists diagnose the disorder through careful evaluations to look for the telltale clinical features of Rett syndrome.
Early and accurate diagnosis of Rett syndrome can help ensure that patients and their families receive the optimal treatment and supportive care as soon as possible. However, incorrect or delayed diagnosis of Rett syndrome is common, especially since early signs of Rett syndrome in toddlers and children often look similar to signs of other, more common conditions.
When should someone get tested for Rett syndrome?
Rett syndrome is characterized by typical development in early life. Babies with Rett syndrome will usually hit early developmental milestones, but development will stall and then regress around age 6 months to 18 months. Infants and toddlers typically lose previously acquired skills, such as crawling or using their hands. If this happens, families are advised to talk to their healthcare providers to investigate potential causes, which may include testing for Rett syndrome.
The first step in a Rett syndrome diagnosis is usually a careful evaluation where a clinician will examine the patient and discuss their developmental history with parents and caregivers to look for signs of Rett syndrome. In many cases, general practitioners will refer families to a Rett syndrome specialist, such as a pediatric neurologist, who will confirm the diagnosis.
Some specific changes that may determine when to test for Rett syndrome include:
- a reduction in spoken language, such as babbling less
- loss of motor skills, such as losing the ability to grasp things with the hands or purposefully reach for objects
- the appearance of unusual hand movements
- trouble walking or abnormal gait patterns, such as being unsteady or walking on toes
- a slowing of head growth
How is Rett syndrome diagnosed?
Rett syndrome is a clinical diagnosis – in other words, doctors diagnose it by observing the signs and symptoms that a patient has experienced and ruling out other potential causes.
Rett syndrome is defined by normal development in early life, then a period of regression followed by recovery or stabilization as patients stop losing skills and possibly even gain some back. According to current Rett syndrome diagnostic criteria, the patient must have experienced this pattern of abnormal development for a diagnosis to be made.
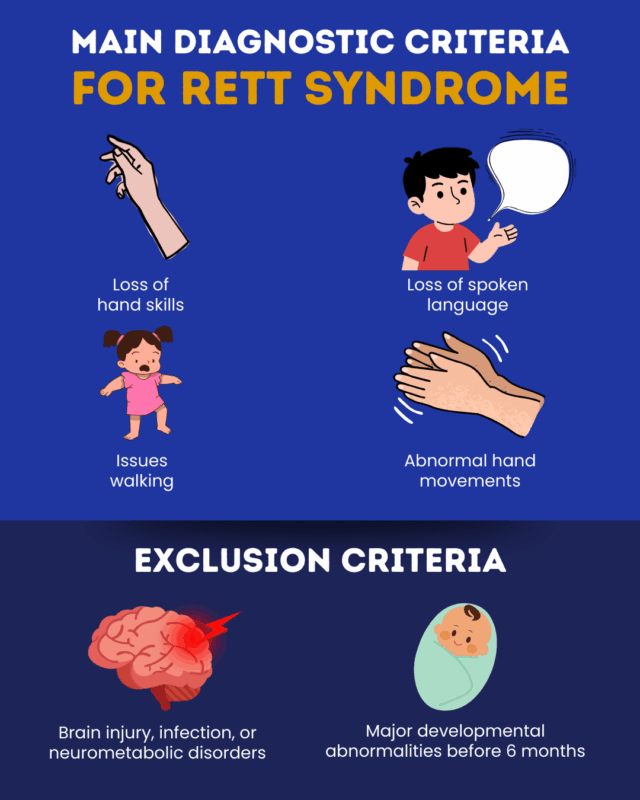
For a diagnosis of typical Rett syndrome to be confirmed, a patient must meet the following four main criteria:
- partial or complete loss of purposeful hand skills like grasping, reaching, and pointing
- partial or complete loss of spoken language, such as losing the ability to say specific words or babbling less
- problems walking, which can range from abnormal gait patterns to a complete inability to walk
- repetitive hand movements such as squeezing, clapping, tapping, bringing the hands to the mouth, or rubbing the hands together
Diagnosing Rett syndrome also requires ruling out other disorders that can cause similar symptoms, which is known as making a differential diagnosis. To confirm a diagnosis of typical Rett syndrome, the following two exclusion criteria must be met:
- the patient does not have a history of brain injury, metabolic diseases affecting the nervous system, or infections that can cause neurological problems
- the patient did not show obvious signs of abnormal development in the first six months of life, such as missing early milestones like being able to swallow or hold the head up.
Diagnosing atypical or variant forms
Most people with Rett syndrome have the typical form of the disease and will meet all the diagnostic criteria listed above. However, some people with Rett syndrome meet most, but not all, of the typical diagnostic criteria. This is referred to as atypical or variant Rett syndrome.
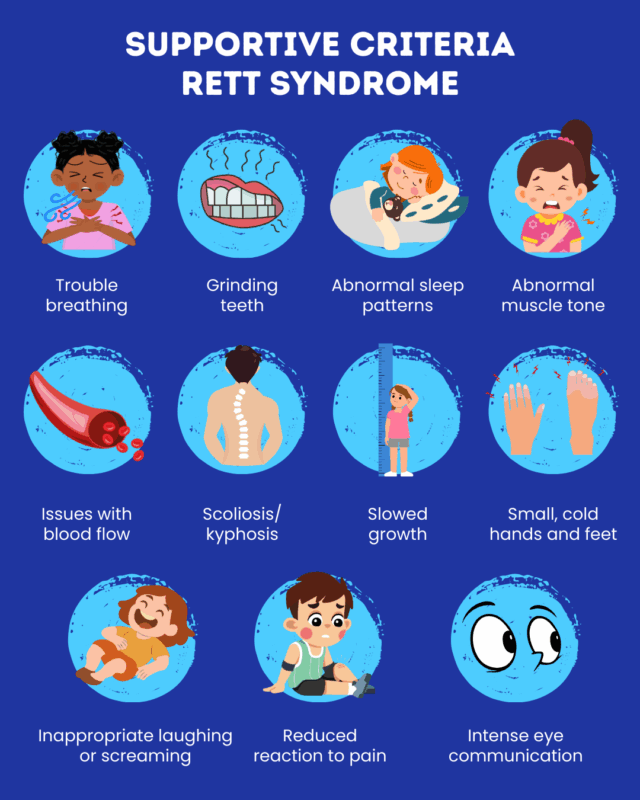
To confirm an atypical Rett syndrome diagnosis, the individual must have shown a Rett-like pattern of normal development, followed by regression, then relative recovery or stabilization. The patient also must meet at least two of the four main criteria for typical Rett syndrome, as well as meet at least five of the following 11 supportive criteria:
- difficulty breathing when awake
- grinding teeth (bruxism) while awake
- abnormal sleep pattern
- abnormal muscle tone
- issues with blood flow in the legs
- scoliosis and/or kyphosis, which are forms of atypical curvature of the spine
- unusually slowed growth
- small, cold hands and feet
- inappropriate screaming or laughing
- a reduced reaction to pain
- intense eye communication, such as using the eyes to point
Genetic testing
In most cases, Rett syndrome is caused by mutations in the MECP2 gene. Some atypical cases of Rett syndrome are associated with mutations in other genes, such as CDJK5 and FOXG1. However, disorders caused by these mutations are now usually classified as distinct from Rett syndrome.
Testing for an MECP2 mutation may help in confirming Rett syndrome in patients displaying disease-typical changes in development. Rett syndrome genetic testing is typically done on a blood sample.
Although most Rett patients have an identifiable mutation in MECP2, some people with a mutation in this gene may not develop the known clinical features of Rett. Examples include females with the familial form of Rett who remain asymptomatic, boys with severe neonatal-onset encephalopathy (marked by profound abnormalities at birth), and people with other neurodevelopmental conditions, such as autism and non-specific intellectual disability.
Additionally, children younger than 3 who have a MECP2 mutation but have not displayed signs of regression or loss of skills are considered to have possible Rett syndrome. If regression occurs, this may be revised to definite Rett syndrome, but if no regression is evident by about age 5, Rett syndrome may not be an appropriate diagnosis.
In the vast majority of cases, Rett syndrome is sporadic, caused by mutations that develop randomly in people with no family history of the disease. There are also a few rare cases where Rett syndrome is hereditary and affects multiple people in the same family. In those instances, genetic testing may help by informing families of the risk of having biological children with the condition.
Next steps after diagnosis
After a diagnosis of Rett syndrome is confirmed, clinicians will work with families to come up with a care plan for the future. This may include:
- Daybue (trofinetide), the only medication approved for Rett syndrome in the U.S., which is indicated to treat patients ages 2 and older and has been shown to help improve communication and ease behavioral issues
- physical therapy, which aims to strengthen the body to improve motor function and coordination
- occupational therapy, which focuses on developing strategies to navigate day-to-day life
- speech therapy, which can aid in communication and eating
- other types of supportive care, such as hippotherapy, hydrotherapy, and music therapy
- considering participation in clinical trials of experimental Rett treatments
Receiving a diagnosis of a lifelong condition can take a substantial toll on families affected by Rett syndrome, but no one needs to navigate life with Rett alone. Several organizations offer support for Rett families, including:
- International Rett Syndrome Foundation
- Girl Power 2 Cure
- Rett Syndrome Research Trust
- Rett Syndrome Angels
Rett Syndrome News is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Recent Posts
- FDA approves Daybue Stix, drug’s powdered formulation, for treating Rett
- My youngest daughter has now lived longer than her older sister did
- Severe epilepsy increases care needs for people with Rett
- Gene therapy NGN-401 leads to functional gains in Rett syndrome
- New study links Rett energy problems to specific gene mutations
- A Rett syndrome clinical trial was our way of paying it forward
- Partners to design AI-based gene editing therapies for Rett
- Rett gene therapy trial starts dosing patients
- Iron-fueled death of cells may drive Rett syndrome damage: Study
- How Rett syndrome affected my children’s birth order traits