New MECP2 Mutation May Lead to Atypical Rett Syndrome, Case Study Reports
Written by |
A newly identified mutation in the MECP2 gene — which is linked to Rett syndrome — was found in two females in Germany who lacked all the common symptoms of the disorder, suggesting these are two cases of atypical Rett syndrome.
The report, “Novel MECP2 Mutation c.1162_1172del; p.Pro388* in Two Patients with Symptoms of Atypical Rett Syndrome,” was published in the journal Molecular Syndromology.
Rett syndrome is a rare neurodevelopmental disorder that affects females almost exclusively. It is characterized by normal early development followed by stagnation, regression, and loss of motor and communication skills between 6 to 18 months of age.
Patients also often show intellectual disability, seizures, poor movement coordination, microcephaly (unusually small head for a given age and gender), and repetitive hand movements.
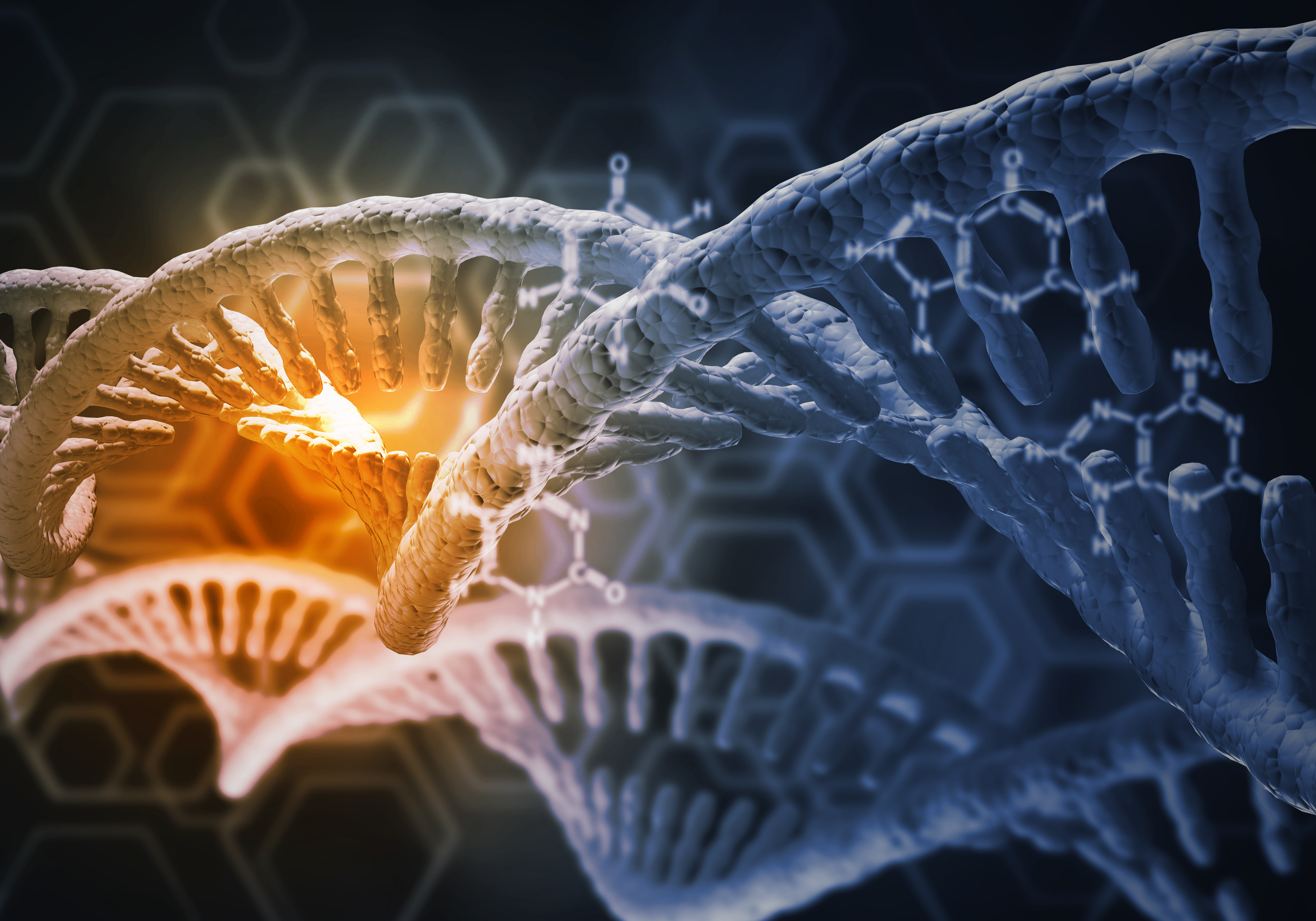
Almost all cases of Rett syndrome are caused by mutations in the MECP2 gene located on the X chromosome (one of the sex chromosomes). This gene provides instructions to produce the MeCP2 protein, which is involved in the growth of nerve cells and the transmission of chemical signals between them.
A total of 30% of Rett patients are estimated to have atypical forms of Rett syndrome, in which their symptoms do not meet all of Rett’s diagnostic criteria. Several subtypes of atypical Rett syndrome have been identified and associated with mutations in MECP2 or other genes.
Researchers in Germany have now identified a new MECP2 mutation in two females — a girl and a woman — with only two typical Rett symptoms: intellectual disability and seizures.
The first patient was an 11-year-old girl whose motor developmental delay was noticed at around 6 months of age. Later, she developed speech delay and behavioral abnormalities, which eased with risperidone, an antipsychotic medicine. Seizures, which started at age 10, were temporarily stopped by treatment with lamictal (lamotrigine).
The second was a 34-year-old woman who showed delayed motor skills, but whose speech progressed normally. She later developed severe intellectual disability and treatment-resistant seizures (at 14 years).
Besides these two typical Rett symptoms, both patients were obese since early childhood and had macrocephaly (overly large head sizes for a given age and gender) and precocious (early) puberty. They also had prominent eyebrows, short necks, and short and plump fingers.
Increasing evidence suggests that Rett patients are at a higher risk of obesity, mainly associated with hyperphagia (excessive hunger). The young girl had excessive hunger, but the woman did not.
Genetic analysis found a new mutation in the MECP2 gene (c.1162_1172del; p.Pro388*) in both patients. This mutation was predicted to be disease-causative, resulting in a premature stop in protein production and leading to a shorter MeCP2 protein that lacks part of a specific region called C-terminal.
MeCP2’s C-terminal region was shown to be critical for interacting with other molecules involved in the regulation of other genes, likely explaining the disease-causative nature of this variant.
Genetic analysis in the young girl had ruled out Temple syndrome, Prader-Willi syndrome, and macrocephalic syndrome, while it showed that the woman did not have the MECP2 mutation in all her cells — an event called mosaicism.
Previous studies have reported cases of mosaic mutations in Rett patients, and a recent study suggested that genetic screening for mosaic mutations may help in understanding Rett’s development and severity.
The patients’ parents had normal weight, were unaffected by the disorder, and did not carry the MECP2 mutation, highlighting that the mutation was not inherited but appeared for the first time in these two people.
Other cases of people with mutations in MeCP2’s C-terminal region and atypical Rett symptoms have been reported, suggesting a potential association between alterations in the C-terminal and atypical forms of the disease.
“This mutation might lead to an atypical Rett syndrome … [but] to substantiate this hypothesis, more clinical cases are needed,” the researchers wrote.
They added that studies on the shorter MeCP2 protein resulting from this mutation are required to understand its implication in abnormal gene regulation and disease development.