X Chromosome Inactivation Not the Only Contributing Factor for Disease Severity in Female Rett Patients, Study Contends
Written by |
The pattern of X chromosome inactivation in female patients with Rett syndrome is not the only contributing factor for disease severity, a study contends.
The research, “X chromosome inactivation does not necessarily determine the severity of the phenotype in Rett syndrome patients,” was published in Scientific Reports.
Rett syndrome is a rare genetic disorder that affects girls almost exclusively and is characterized by developmental and intellectual disabilities.
The condition is caused by mutations in the MECP2 gene (located on the X chromosome) that provides instructions to make a protein called MeCP2. This protein is responsible for maintaining synapses, which are the junctions between nerve cells that allow them to communicate.
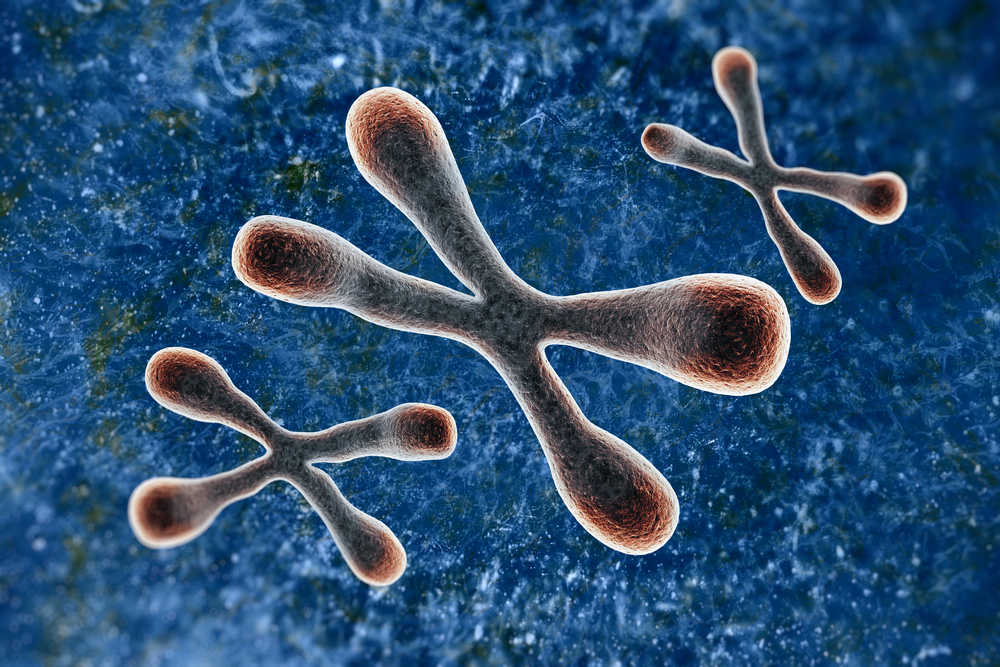
Women carry two X chromosomes — one from the mother and one from the father — while men carry only one, inherited from the mother. To ensure that all genes in the X chromosome are expressed equally in men and women, a process known as X chromosome inactivation takes place during embryonic development, at which time one of the two X chromosomes carried by females is randomly selected to be inactivated.
Since the discovery in 1999 that Rett syndrome is caused by genetic defects in the MECP2 gene, more than 800 different mutations — some with more debilitating effects than others — have been documented. According to the authors, “these clinical differences have been attributed, at least in part, to X chromosome inactivation (XCI).”
“Since MECP2 is located on the X chromosome, the severity of [Rett syndrome] could be theoretically regulated by XCI,” they argued. In this scenario, patients with more severe symptoms would be those in which the X chromosome left active in most of their cells contained the mutated MECP2 gene.
“[H]owever, classical methylation-based protocols to evaluate XCI could not determine whether the preferentially inactivated X chromosome carried the mutant or the wild-type [normal] allele [variants of the same gene],” the investigators explained.
(Of note, methylation is a chemical modification in which a methyl group is added to the DNA sequence of a gene or several genes, inactivating them. With standard methylation-based protocols it is possible to identify which X chromosome has been inactivated by XCI, based on the methylation pattern of its genes.)
In this study, a group of Spanish researchers developed a new method that allowed them to analyze the methylation pattern of a region within the X chromosome where several MECP2 mutations have been observed.
Using the new method, investigators now could tell which X chromosome — the one that remained active after XCI, or the one that was inactivated — contained the mutated MECP2 gene, and set out to test whether XCI might be related to disease severity.
They performed the new protocol on blood samples that had been collected from 174 female Rett syndrome patients carrying nine different genetic mutations in MECP2.
In most cases, they found XCI happened randomly — sometimes affecting the X chromosome containing the mutated MECP2 gene, or the other containing a normal version of the gene — and failed to find a clear relationship between XCI and the severity of the symptoms presented by each patient.
They also compared the methylation patterns of the X chromosome in blood and brain samples that had been obtained from two patients who died, and discovered the XCI patterns in both tissues were different.
“However, [Rett syndrome] mainly being a neurological disease complicates the establishment of a correlation between the XCI in blood and the clinical presentation of the patients,” they wrote.
Finally, researchers measured the levels of MECP2 gene transcripts (the molecules that serve as templates for the production of a protein) and found them to be different from those they were expecting to see based on the XCI patterns.
Essentially, this means that “[m]any factors other than XCI could affect the [Rett] phenotype [disease presentation], which in combination could influence the clinical presentation of [Rett] patients to a greater extent than slight variations in the XCI pattern.”
“[O]ur results show that the relationship between XCI and the severity of the [Rett] phenotype is not straightforward. Factors other than XCI can influence MECP2 transcript levels, and presumably many additional factors, such as genetic polymorphisms [variations] and the expression of other genes, may influence the final clinical presentation of RTT,” the researchers concluded.